Atherosclerosis Overview
Coronary heart disease (CHD) is a narrowing of the small blood vessels that supply blood and oxygen to the heart. CHD is also called coronary artery disease (CAD).
(CHD) is considered as one of the leading causes of deaths and hospital admissions for men and women all over the world.
 (CHD) is caused by the buildup of plaque in the arteries to the heart. This may also be called hardening of the arteries.
(CHD) is caused by the buildup of plaque in the arteries to the heart. This may also be called hardening of the arteries.
Fatty material and other substances form a plaque build-up on the walls of the coronary arteries. The coronary arteries bring blood and oxygen to the heart.
This buildup causes the arteries to get narrow and even narrower over time.
As a result, blood flow to the heart can slow down or stop (the heart attack).
A risk factor for heart disease is something that increases the chance of getting it. You cannot change some risk factors for heart disease, but others you can change.
The risk factors for heart disease that you CANNOT change are:
The age, the risk of heart disease increases with age.
The gender, Men have a higher risk of getting heart disease than women who are still getting their menstrual period. After menopause, the risk for women is closer to the risk for men.
The genes, if the parents or other close relatives had heart disease, the risk is higher.
The race, African Americans, Mexican Americans, American Indians, Hawaiians, and some Asian Americans also have a higher risk for heart problems.
Many things increase your risk for developing heart disease:
Diabetes is a strong risk factor for heart disease.
High blood pressure (hypertension) increases the risks of heart disease and heart failure (the weak heart).
Extra cholesterol in the blood builds up inside the walls of your heart’s arteries (blood vessels).
Smokers have a much higher risk of heart disease.
Chronic kidney disease can increase the risk.
People with narrowed arteries in another part of the body (examples are stroke and poor blood flow to the legs) are more likely to have heart disease.
Substance abuse (such as cocaine)
Being overweight
Not getting enough exercise and feeling depressed or having excess stress are other risk factors.
Symptoms may be very noticeable, but sometimes you can have the disease and not have any symptoms.
Chest pain or discomfort (angina) is the most common symptom. The feel this pain when the heart is not getting enough blood or oxygen. How bad the pain is varies from person to person.
It may feel heavy or like someone is squeezing the heart. It could be felt under the breast bone (sternum), also in the neck, arms, stomach, or upper back.
The pain usually occurs with activity or emotion, and goes away with rest or a medicine called nitroglycerin.
Other symptoms include shortness of breath and fatigue with activity (exertion).
Women, elderly people, and people with diabetes are more likely to have symptoms other than chest pain, such as:
Fatigue
Shortness of breath
Weakness
Many tests help diagnose CHD. Usually, your doctor will order more than one test before making a diagnosis.
Tests may include:
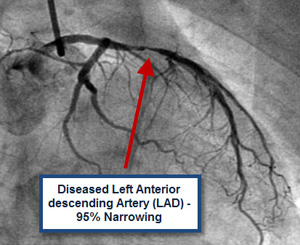
Coronary angiography/arteriography — an invasive test that evaluates the heart arteries under x-ray
CT angiography — a noninvasive way to perform coronary angiography
 Echocardiogram
Echocardiogram
Electrocardiogram (ECG)
Exercise stress test
Heart CT scan
Magnetic resonance angiography
Nuclear stress test
You may be asked to take one or more medicines to treat the blood pressure, diabetes, or high cholesterol levels. Follow your doctor’s directions closely to help prevent coronary artery disease from getting worse.
Goals for treating these conditions in people who have coronary artery disease:
Blood pressure less than or equal to 140/90 (even lower for some patients with diabetes, kidney disease, or heart failure)
Glycosylated hemoglobin (HbA1c) levels less than or equal to 7% for people with diabetes
LDL cholesterol level less than or equal to 100 mg/dL (even lower for some patients)
Treatment depends on your symptoms and how severe the disease is. Your doctor may give you one or more medicines to treat CHD.
NEVER ABRUPTLY STOP TAKING ANY OF THESE DRUGS. Always talk to your doctor first. Stopping these drugs suddenly can make the angina worse or cause a heart attack.
The doctor may refer you to a cardiac rehabilitation program to help improve your heart’s fitness.
Procedures and surgeries used to treat CHD include:
Angioplasty and stent placement, called percutaneous coronary interventions (PCIS)
Coronary artery bypass surgery
LIVE A HEALTHY LIFESTYLE
Some of the risks for heart disease that you CAN change are:
Do not smoke or use tobacco.
Get plenty of exercise, at least 30 minutes a day on at least 5 days a week (talk to your doctor first).
Maintain a healthy weight. Men and women should aim for a body mass index (BMI) between 18.5 and 24.9.
If you drink alcohol, limit yourself to no more than one drink per day for women, and no more than two drinks per day for men.
Nutrition is important to your heart health, and it will help control some of your heart disease risk factors:
Choose a diet rich in fruits, vegetables, and whole grains.
Choose lean proteins, such as chicken, fish, beans, and legumes.
Eat low-fat dairy products, such as low-fat milk and low-fat yogurt.
Avoid sodium (salt) and fats found in fried foods, processed foods, and baked goods.
Eat fewer animal products that contain cheese, cream, or eggs.
Read labels, and stay away from “saturated fat” and anything that contains “partially-hydrogenated” or “hydrogenated” fats. These products are usually loaded with unhealthy fats.
In-Depth Treatment
Everyone recovers differently. Some people can maintain a healthy life by changing their diet, stopping smoking, and taking medications exactly as the doctor prescribes. Others may need medical procedures such as angioplasty or surgery.
Although everyone is different, early detection of CHD generally results in a better outcome.
When to Contact a Medical Professional
If you have any risk factors for CHD, contact your doctor to discuss prevention and possible treatment.
Immediately contact your health care provider, call the local emergency number, or go to the emergency room if you have:
Angina or chest pain
Shortness of breath
Symptoms of a heart attack
Dr. Ehab M. Esheiba
MBBCh, DM, MSc (Cardiology), MRCP (UK), MRCP (London).
Lecturer & Specialist in Cardiology.
Gulf Medical College Hospital & Research Centre.
Gulf Medical University.

